Study
Elham Kazemian, Ali Pourali, Fatemeh Sedaghat , Mehrdad Karimi, Vahid Basirat, Zohreh Sajadi Hezaveh, Sayed Hossein Davoodi, Michael F Holick (2023)
https://doi.org/10.1093/nutrit/nuac068
This meta-analytical study assessed the impact of vitamin D3 supplementation on bone health of different skeletal areas. Vitamin D supplementation showed to significantly increase bone mineral density at the lumbar spine, femoral neck and total hip. These alterations were positively correlated with the vitamin D dose (400 – 7000. I.U./day), indicating higher vitamin D doses were linked to a higher BMD. Furthermore, proper vitamin D supplementation is demonstrated in this study to alter bone turnover markers like PTH.
BACKGROUND
Vitamin D deficiency, a widespread condition in the global population*, is associated with loss of bone mineral density and increased bone turn over events. Bone mineral density and bone turnover markers remain as one of the most relevant parameters, to properly assess bone health and osteoporotic clinical pictures. By utilizing these biomarkers, patients can be accessibly monitored during osteoporosis treatment for assessment of therapy effectiveness, prediction of fracture risks and also long-term stability of implants. Due to the fact, that vitamin D is an integral part of the calcium absorption process and ultimately contributes to bone mineralization, the steroid hormone is already an established nutrient in the osteoporosis treatment.
AIM
The study aimed to assess the outcomes of a vitamin D supplementation on bone mineral density and bone turn over markers. For this, 39 studies with a total of 9527 participants were included for the systematic review and meta-analysis. The applied vitamin D dose ranged from 300 – 10.000 I.U, most of the studies offered the patients vitamin D on a daily basis (alternative was weekly or monthly). The duration of the trials ranged from 3 months to 5 years. Bone mineral density and bone turn over markers (e.g. PTH) were measured during the trials. Mean baseline 25(OH)D concentration was 21,08 ng/ml in the intervention groups and 21,28 ng/ml in the control groups.
RESULTS
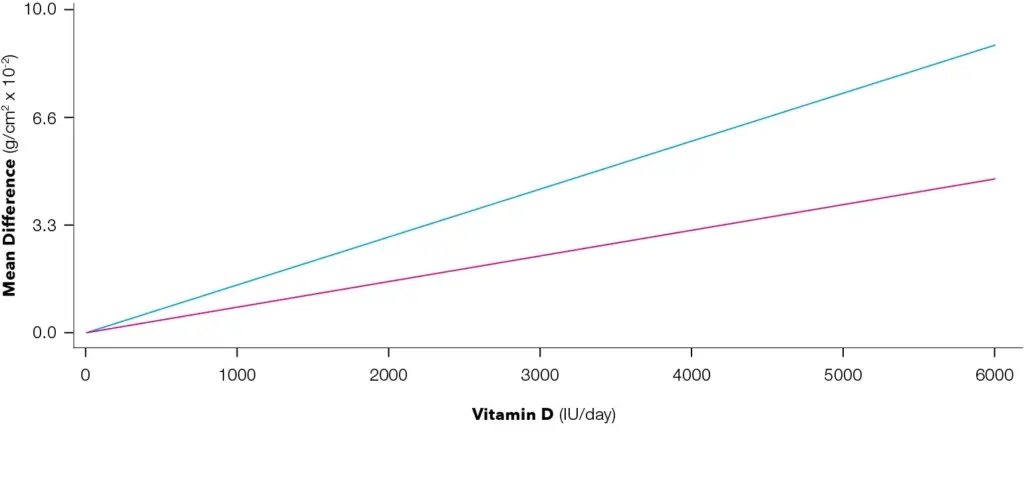
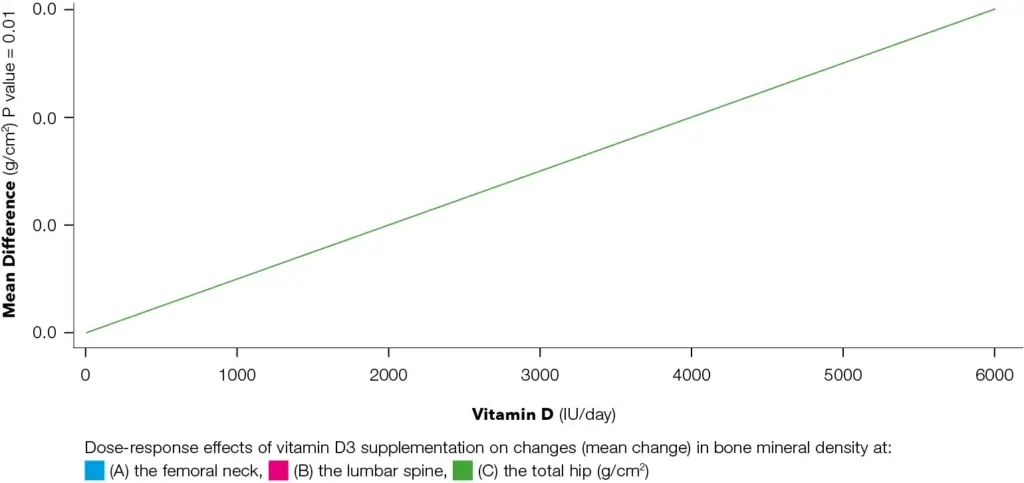
Administration of vitamin D supplements lead to an average 25(OH)D concentration change of 18,88 ng/ml in the intervention groups and a 2,16 ng/ml change in the control group, highlighting, that frequent vitamin D supplementation is able to positively alter and increase vitamin D levels. All patients from the intervention groups after receiving vitamin D supplements exceeded 20 ng/ml in all studies, showcasing the positive effect of supplementation on the 25(OH)D concentration, whereas the control groups in the majority of the studies were still below 20 ng/ml, which equals vitamin D deficiency. Furthermore, the intervention groups receiving vitamin D supplements showed to have significantly altered bone mineral densities at the lumbar spine, femoral neck and total hip compared to the control group. The administered vitamin D doses were positively linked to increased bone mineral densities at the relevant skeletal sides, highlighting a dose-dependent response with a linear relationship (lumbar spine, femoral neck, total hip). There were no significant changes detected for the total body or trochanter sites in terms of bone mineral density. Patients receiving supplementation were observed to have increased vitamin D levels and decreased bone turn over markers (PTH, DPD).
CONCLUSION
The outcome and evaluation of the systematic review underlines the skeletal benefits of vitamin D supplementation by significantly influencing the bone mineral density in the lumbar spine, femoral neck and total hip sites. Additional factors like ethnicity, menopause status and also age have shown to be relevant parameters, underlining the need for further differentiated study populations. Taken together, vitamin D supplementation has shown to have protective effect for bone mineral density, a key factor also in the dentistry field, since it enables proper implant placements and long-term stability.
*Amrein et al., 2020; Forrest & Stuhldreher, 2011; Siddiqee et al., 2021










