CASE OF THE MONTH | 03/2025
INITIAL SITUATION
A 36-year old female patient in good general health presented with a history of a traumatic experience when 12 years old associated to the upper left lateral incisor tooth. The tooth subsequently became ankylosed, discoloured and a step deformity developed over time. The tooth was not root treated, and upon presentation was clearly being affected by internal resorption.
TREATMENT PLANNING
Tooth 22 was clearly beyond saving and had previously been splinted following orthodontic treatment to maintain stability. The female patient had a very high smile line (something that would likely become higher following successful treatment) which meant treatment modalities had to be carefully planned and executed to ensure aesthetic success. Tooth 22, already ankylosed with a superior gingival margin had also approximately 2-3mm of gingival recession, so there was a need to manage the volume of keratinised mucosa as part of the treatment process.
Following extensive discussions of all the treatment options possible, the patient requested a fixed implant retained tooth.
We discussed for an optimal aesthetic outcome we would use a removable provisional acrylic denture to replace the missing 22 once extracted with a small pink acrylic buccal flange and tooth of ideal aesthetic proportions. A delayed implant placement approach was chosen to allow significant soft and early hard tissue healing to occur. Guided bone regeneration with cerabone® and Jason® membrane was chosen to provide contour ridge augmentation. After the hard tissue healing phase of 12 weeks, the restorative phase utilising a provisional acrylic crown to develop a fully customised emergence profile was completed.
The patient did not want a space nor did she want a denture long term and fixed bridgework was not appropriate due to a lack of appropriate supporting teeth. We discussed adhesive bridgework, but the patient wanted a fixed tooth solution without the risk of debonding.
The initial phase of treatment helped with the planning of the implant therapy. The upper left lateral incisor tooth was removed atraumatically and an immediate acrylic denture fitted with pink acrylic to demonstrate the loss of the buccal hard and soft tissues.
SURGICAL AND PROSTHETIC PROCEDURE
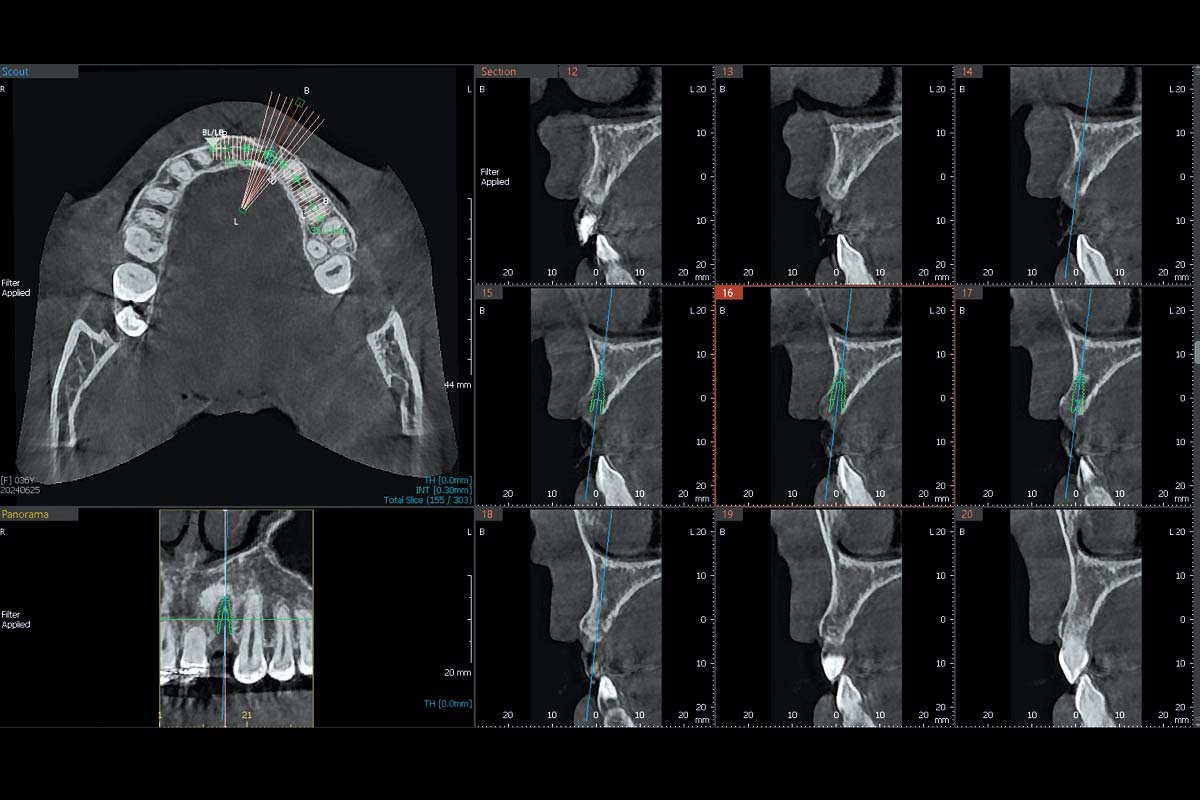
- 8 Weeks after tooth removal the hard tissue volume was reassessed with a CT scan and virtual implant placement planning for a screw retained restoration
- 10 weeks after tooth removal – the soft tissue maturation was excellent and implant placement planned
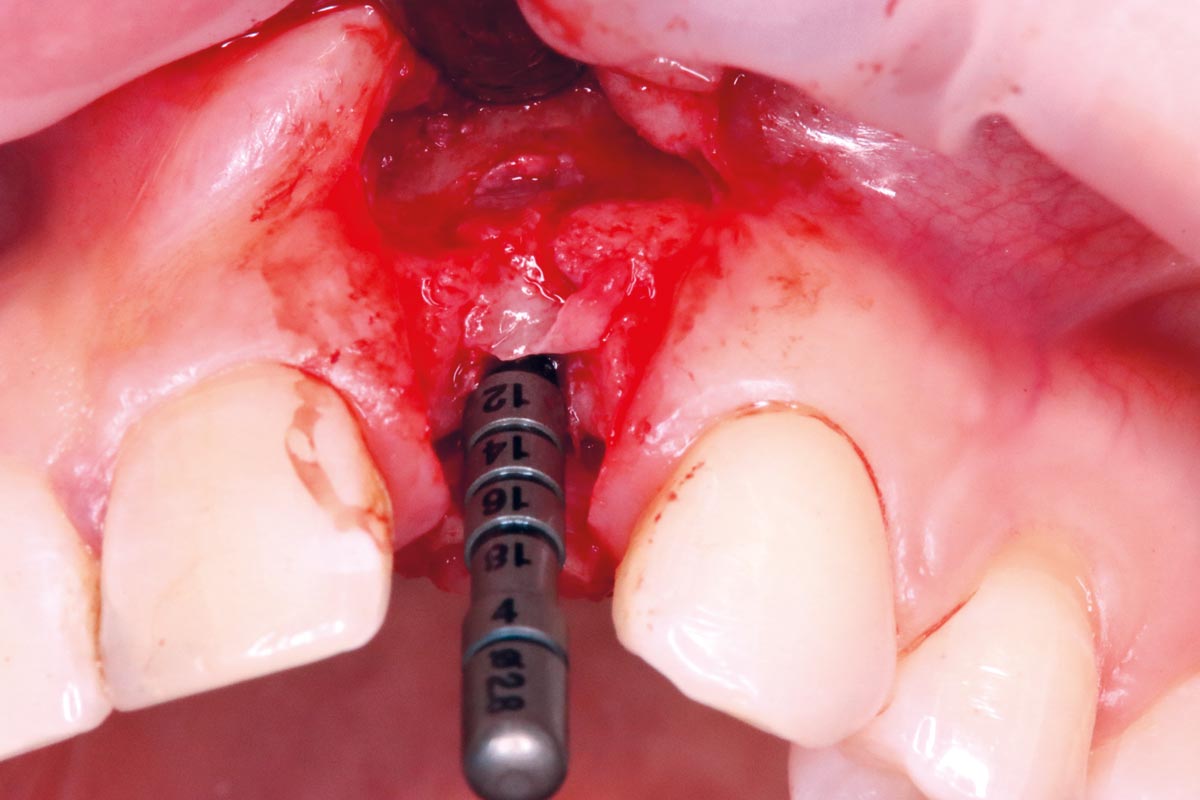
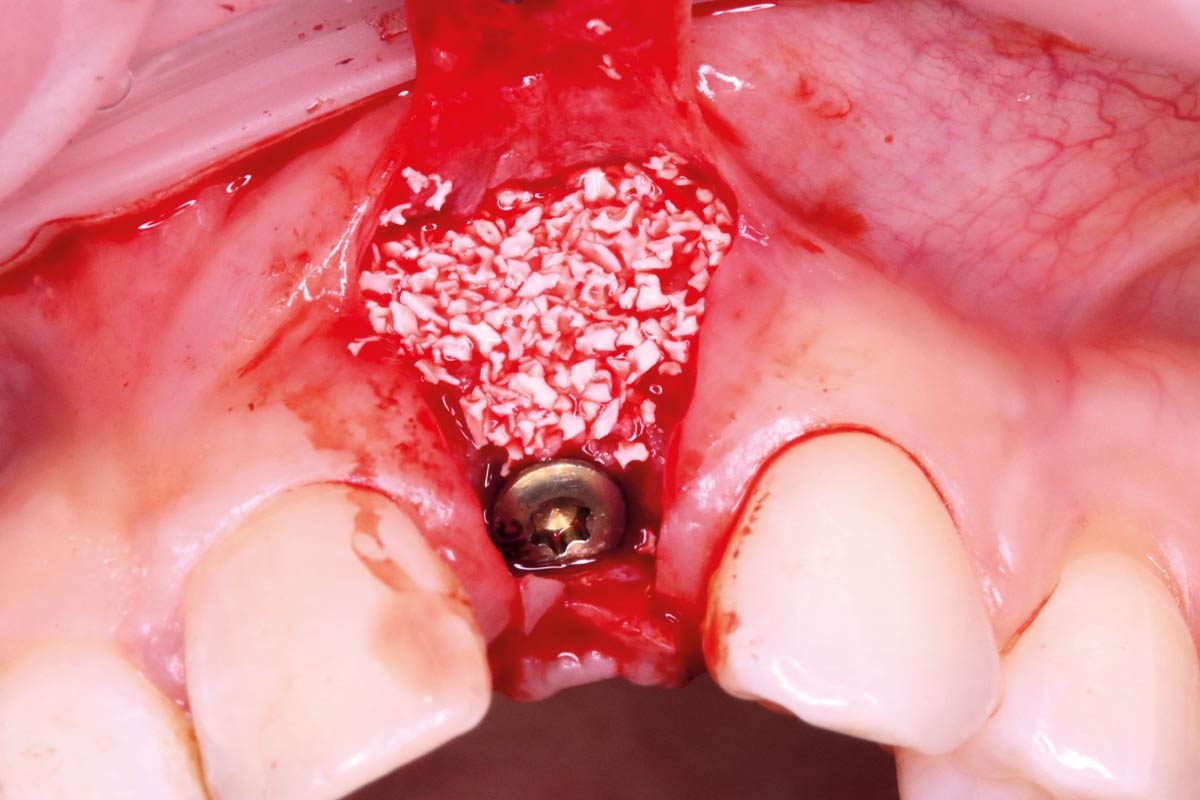
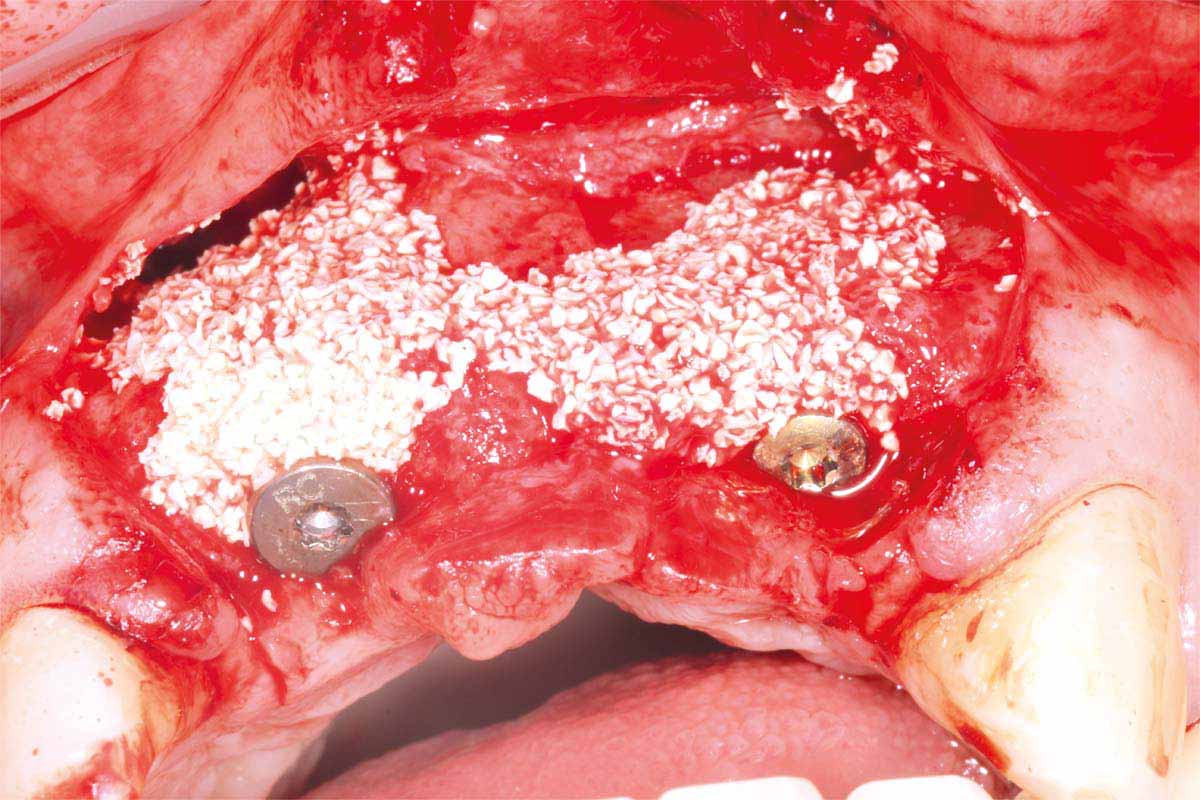
- A papilla sparing full thickness crestal incision was raised with mesial and distal vertical relieving incisions into the sulcus to expose the healing alveolar ridge with early soft bone formation in the socket
- The primary implant osteotomy for a Straumann® Bone Level Tapered Implant (BLT) 3.3mm and a guide pin was used for implant angulation confirmation
- A slower drilling speed of 350rpm was utilized to harvest autogenous bone chips in the flutes of the Straumann® BLT implant drills
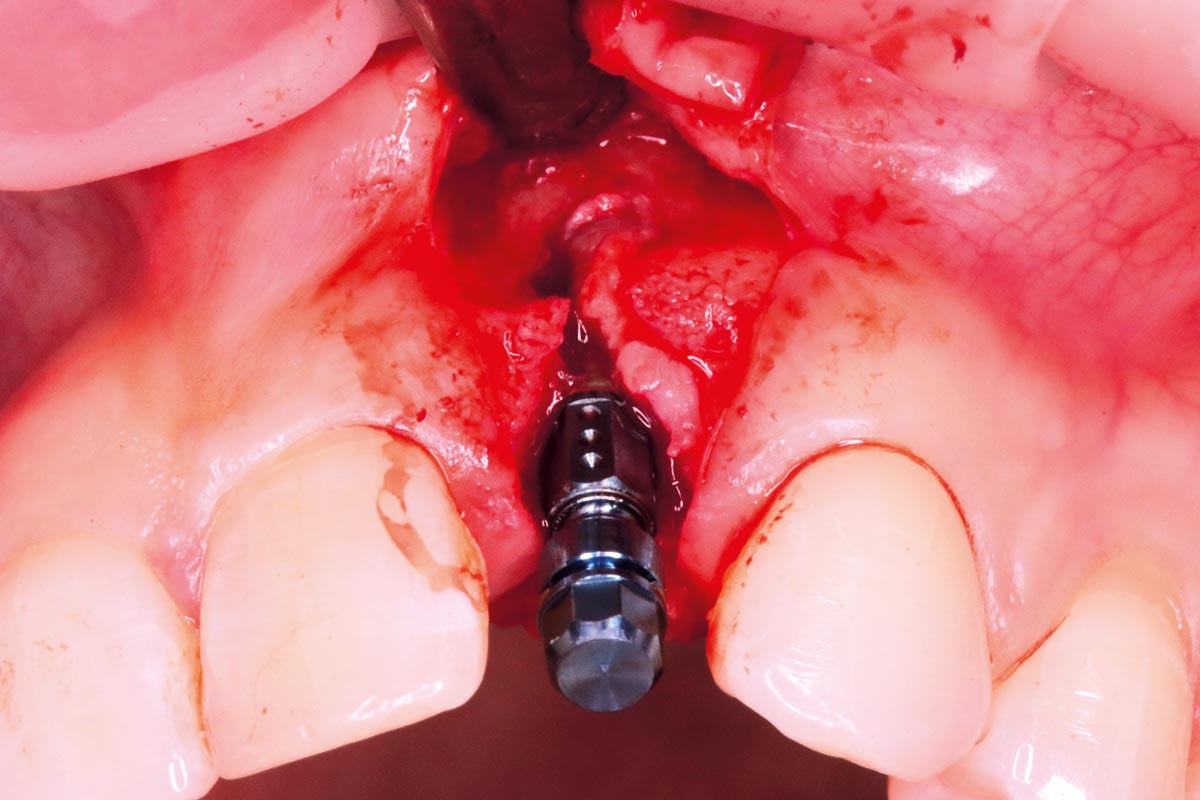
- The 12mm BLT implant fixture was hand positioned in situ
- The BLT implant fixture had thin buccal bone on its surface and this was covered with the collected autogenous bone chips
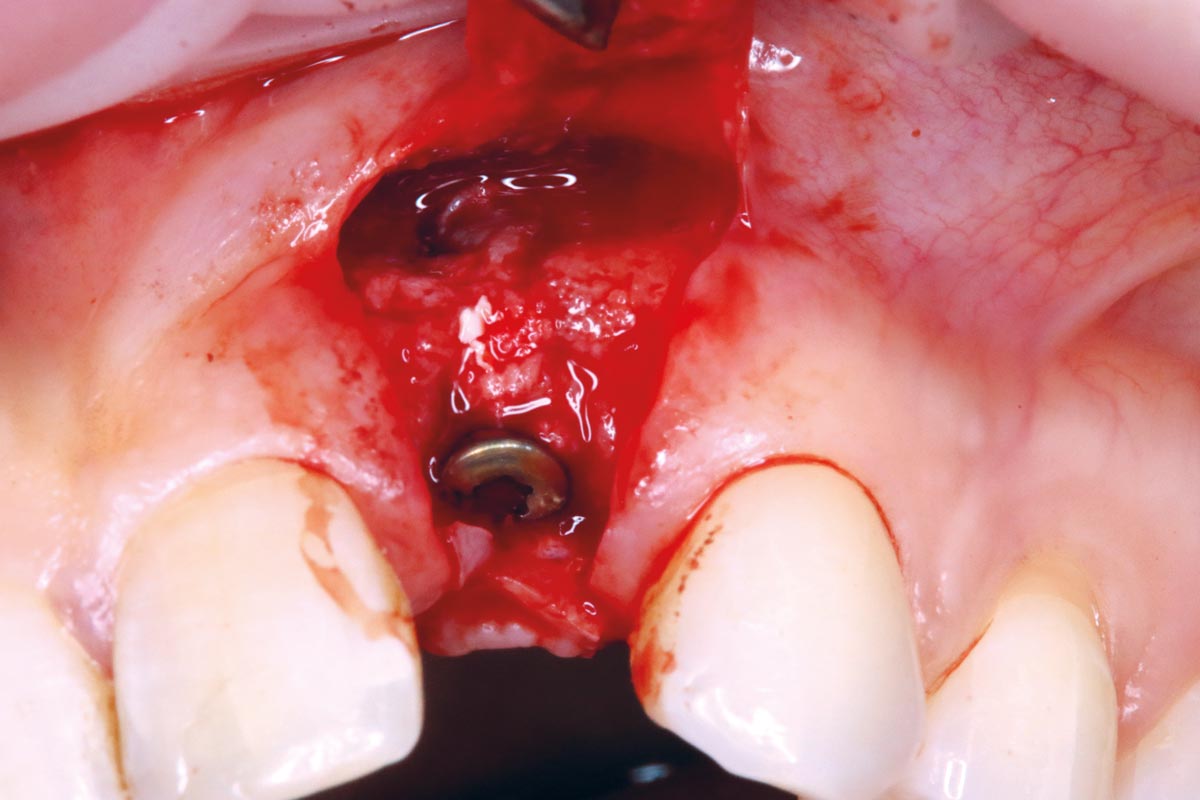
- A 2mm healing abutment was used to “tent” the soft tissues coronally to increase the connective tissue volume
- Then a layer of xenograft to augment the buccal bone volume – cerabone® – was applied
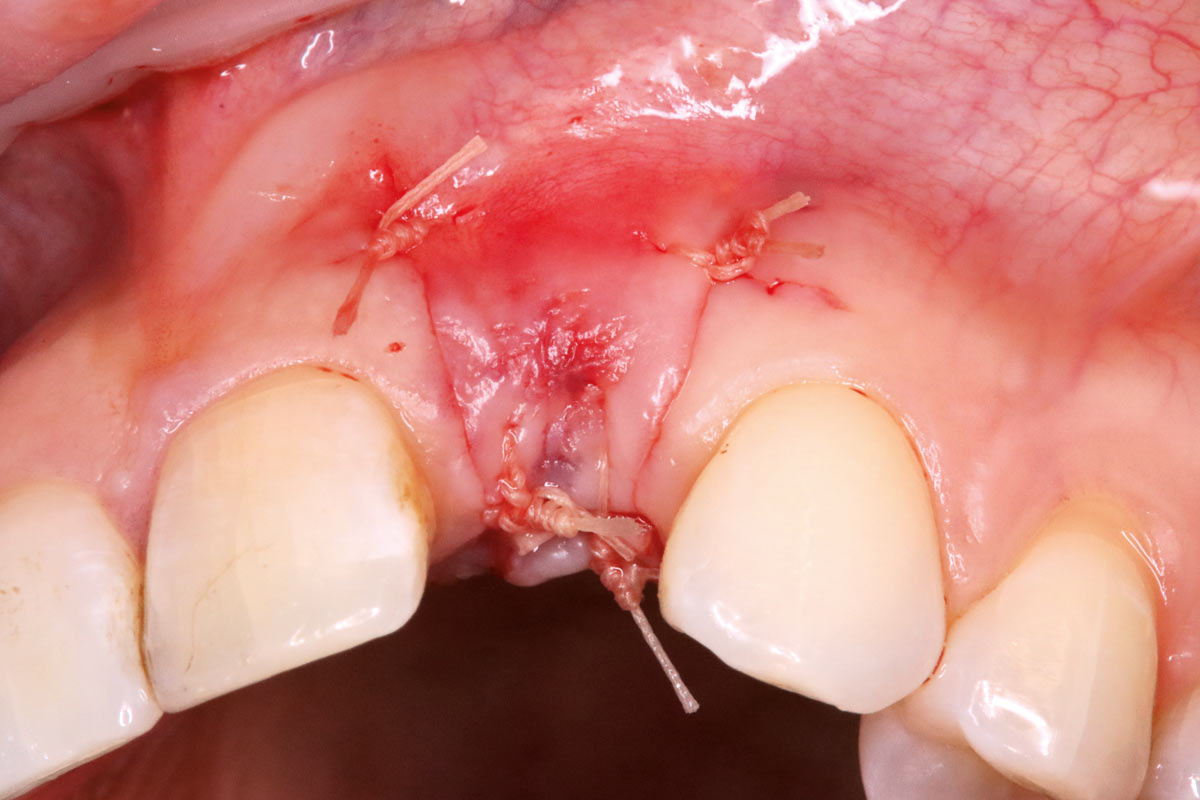
- A porcine collagen membrane was customized for the site – to avoid the flap margins – Jason® membrane
- Excellent passive primary closure of the surgical site was ensured
- The denture was modified to remove the pink buccal acrylic to prevent intrusion into the surgical site
- The postoperative radiograph showed appropriate implant placement
- The surgical site was left to mature for 10 weeks before beginning the restorative phase
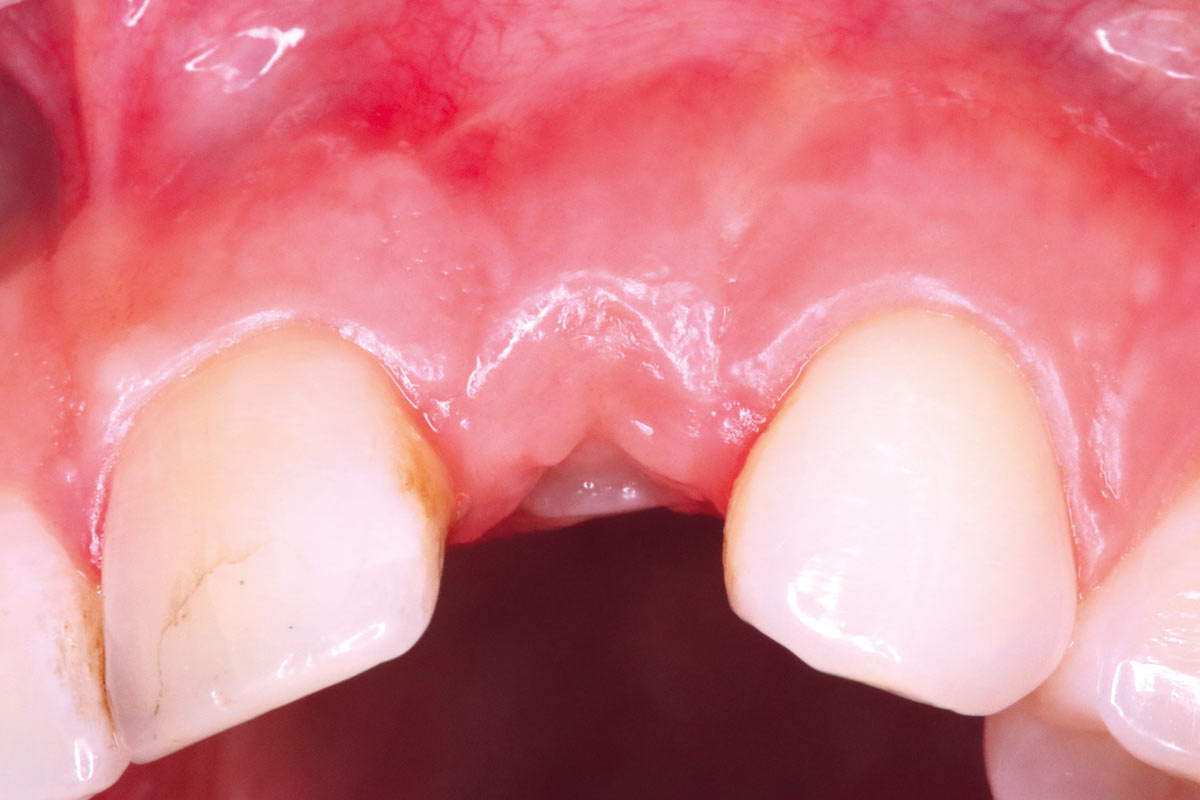
- A small h-shaped incision was made over the fixture head area and a larger wider healing abutment used to widen the soft tissues emergence area
- A monoscanbody was placed and digital 3 shape scan taken for provisional restoration fabrication
- an acrylic provisional crown with its fully customized emergence profile was fabricated
- the acrylic nature allows us to modify if required so that we can adjust the emergence profile chairside with either the addition of composite resin or the modification of the acrylic crown
- a small h shaped incision was made to push/expand the soft tissues when the provisional crown was seated in situ
- following a period of 6 weeks to allow the soft tissue emergence profile to mature the emergence profile was captured with a new 3 shape digital scan and the monoscanbody in situ (but being careful to not allow soft tissue collapse following removal of the acrylic provisional crown)
- the definitive screw-retained ceramic crown was fabricated and subsequently fitted atraumatically 3 weeks later
FINAL RESULT
Following fit of the definitive ceramic crown there was initial soft tissue compression which subsided with loss of the blanching effect. The hard and soft tissue healing was clearly maturing well and the Straumann implant osseointegrating. The papillae mesially and distally were already being supported by the prosthodontic shape of the restorations and contact areas. The volume of keratinised mucosa had regenerated well and the aesthetic outcome very close to optimal.
CONCLUSION
The patient was extremely happy with the aesthetic and functional outcome, having had many years of concern with the tooth following the initial trauma.
Adopting the delayed approach allowed the soft tissue volumes to correct to more anatomical proportions. This meant we could correct the previous gingival recession predictably without the need for any soft tissue grafting procedures avoiding the comorbidities these procedures bring (including further recession over time without the appropriate hard tissue grafting support).
The use of the xenogenic grafting materials – cerabone® and Jason® membrane – allowed a very predictable, very long-term approach to contour ridge augmentation to rebuild the lost buccal profile following tooth removal.
There appeared to be some very superficial small superfluous biomaterial exfoliating through the mucosa at the 6 month review but overall the result appears to be an extremely stable and long-term excellent outcome.
Also interesting
- Dr. Ross CuttsUnited Kingdom
- Dr. Ross CuttsUnited Kingdom
- Dr. Ross CuttsUnited Kingdom