CASE REPORT
The presented case describes the rehabilitation of a challenging extended edentulous site in the posterior lower jaw, using state-of the-art bone regeneration- and soft tissue management techniques, with the goal to bring back the patient a long-term stable dentition.
INITIAL SITUATION
A female patient (66 years old) came to the clinic requesting a periodontal treatment. The patient was in healthy condition, without taking medication and was a non-smoker. She was already missing tooth #36, #37 and #25 (Fig. 1 and 2). After initial periodontal treatment, revaluation and maintenance therapy, the patient requested to restore the missing teeth. The tooth gap at position #36 and #37 impaired the patient’s ability to chew and was therefore primarily of functional concern.
TREATMENT PLANNING
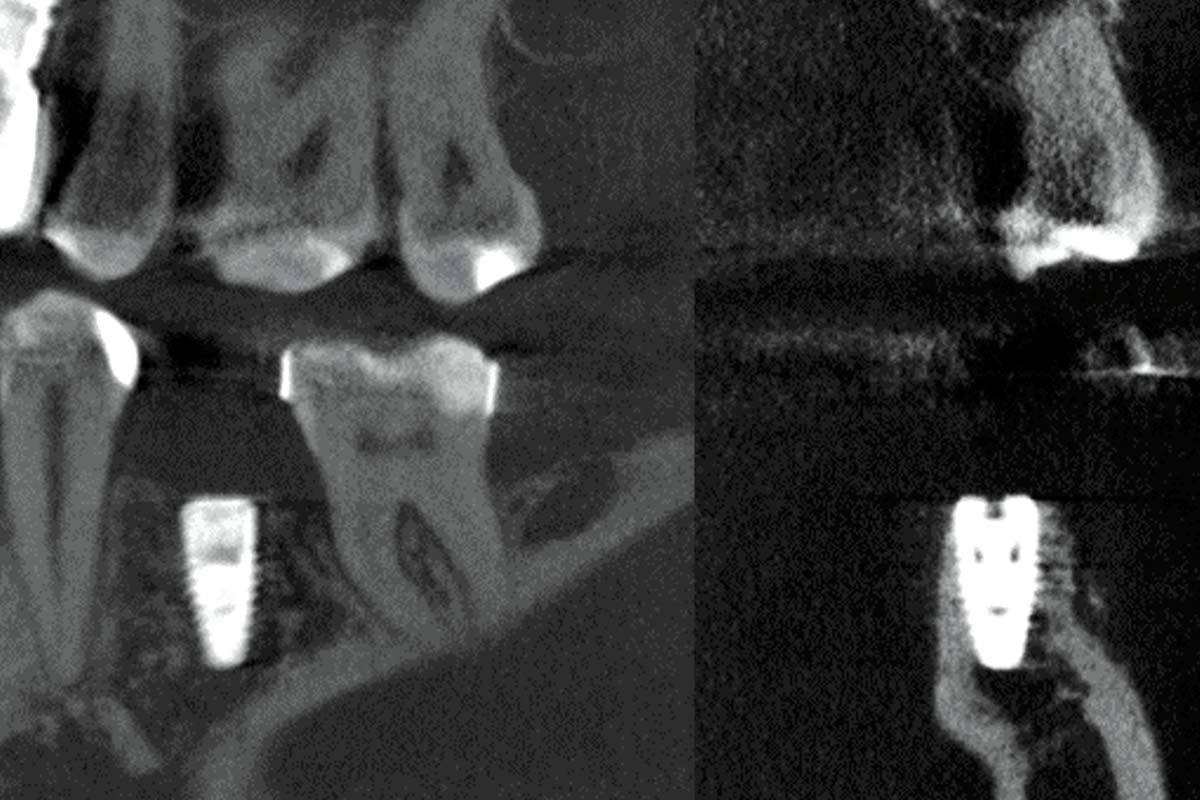
After CBCT assessment (Fig. 3 and 4), implant placement and simultaneous GBR was proposed to the patient. Since three defects were expected to occur around the implant (buccal and lingual dehiscence and a small two to three millimetre vertical defect on the distal side of the implant), a non-resorbable membrane (permamem®) was planned to be used, which would provide sufficient form stability and thus optimal conditions for complete defect resolution. A combination of autogenous graft and a volume stable bone substitute (cerabone® plus) were planned to be used as a bone graft. The autogenous bone would be collected with a bone scraper form the retromolar region adjacent to the defect site. Finally, a soft tissue management procedure will be planned prior to the restorative work.
SURGICAL AND PROSTHETIC PROCEDURE
Implant placement and GBR
A full thickness flap was raised with a vertical incision. The incision was elongated in the distal direction in order to include the retromolar region (Fig. 5). Then the patient underwent an atraumatic extraction of tooth number #38 as the tooth showed a poor perio prognosis with deep pockets and resorption more than half to two-thirds of the root length. Thereafter, a 4.1 x 10 BLT Straumann bone level implant was placed and, as expected, three peri-implant defects were present (Fig. 6 – 8). Cortical perforations were performed on the buccal aspect. The membrane (permamem®, 20 x 30 mm) was trimmed according to the defect size and initially stabilised in the apical part of the membrane. Subsequently a bone graft was placed: for the first layer only autogenous bone was used, which was harvested from the retromolar area (Fig. 9 – 11) and packed around the exposed implant surface (Fig. 12). For the second layer a mixture of 50% autogenous bone and 50% cerabone® plus was used (Fig. 13). The second layer was used on top of the first layer. Afterwards, the membrane was placed over the graft, tightly adapted and completely stabilized with additional bone pins (Fig. 14). 6.0 monofilament resorbable mattress sutures were used to achieve primary and tension-free wound closure (Fig. 15).
Re-entry
After six months of healing time, the treated site presented with excellent soft tissue healing (Fig. 19) and was reopened with a full thickness flap and the non-resorbable membrane was removed (Fig. 16 and 17). The re-entered site showed optimal graft integration with a sufficient bone gain both in horizontal and vertical dimension (Fig. 17 and 18). However, displacement of the mucogingival line and a reduced width of the keratinized mucosa was evident (Fig. 19).
Soft tissue management
Two months after re-entry and membrane removal, a widening of the keratinized mucosa was performed: an apically positioned flap was combined with a free gingival graft. The graft was taken from the distal part of the palate (Fig. 20 – 22).
Two months after the third procedure, a sufficient gain of keratinized tissue could be achieved (Fig. 23 and 24). Then, the implant uncovering procedure was performed with simultaneous peri-implant soft tissue augmentation. In order to avoid a second harvesting procedure from the palate, a porcine acellular dermal matrix (mucoderm®) was used instead. The matrix was hydrated in sterile saline solution and placed at the buccal aspect. The marginal soft tissues were sutured using 6.0 non-resorbable monofilament sutures (Fig. 25 – 27).
Six weeks after healing abutment placement, a provisional crown was fabricated. The provisional crown was used to condition the soft tissue and obtain a more natural emergence profile (Fig. 28 – 31).
FINAL SCORE
A screw retained monolithic ceramic zirconia crown (on Variobase link) was created as definitive restoration (Fig. 32). The bone augmentation procedure allowed the fulfilment of two important goals: 1) prosthetically driven implant placement, which enables fabrication of a screw retained crown and 2) bony walls of adequate thickness (minimum of two millimetres) surrounding the implant. Soft tissue augmentation procedures recreated the peri-implant soft tissue of adequate quality (two millimetres keratinized soft tissue) and thickness (at least two millimetres), which has a positive long-term effect providing peri-implant soft tissue and marginal bone stability and facilitating the maintenance of oral hygiene.
CONCLUSION
The fulfilment of all aforementioned points is especially important in periodontally compromised patients, who have an increased risk for developing peri-implantitis. A detailed clinical diagnosis and treatment planning together with the selection of suitable biomaterials is key for achieving a satisfying outcome both on a functional and aesthetic level.